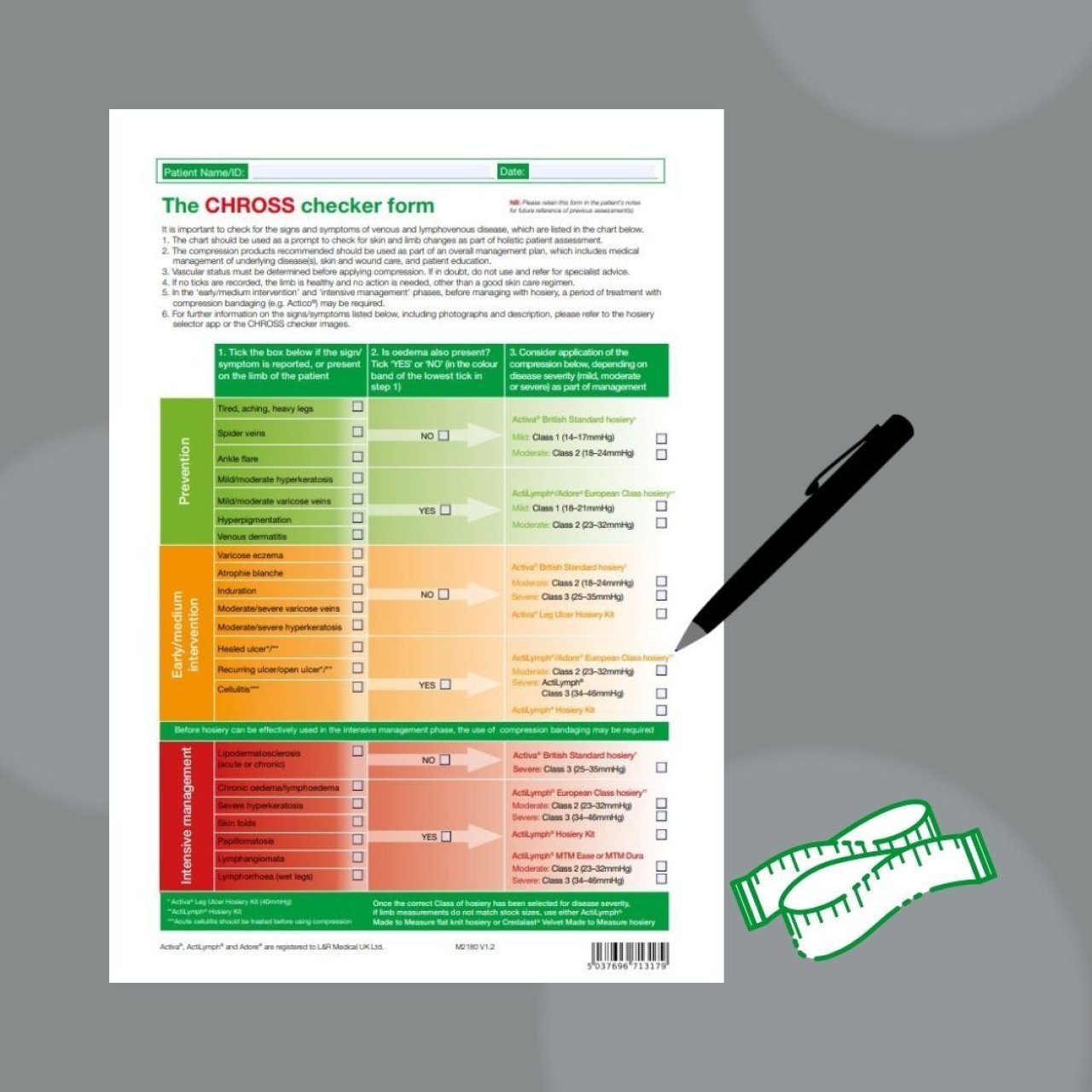
Leg Ulcer Hosiery Kits are an alternative to compression bandaging, delivering full therapeutic compression. They support patient self care, reduces nursing time to care, and eliminates clinical variation in application technique.
Leg ulcer hosiery kits can be used as first-line treatment of venous leg ulcers (VLUs) for patients who have low to moderate wound exudate and minimal limb distortion.
Benefits include:
Optimal 40mmHg compression for effective VLU healing
Simple to apply consistently and safely
Requires minimal training and can be reapplied by the patient, carer and other members of the multi-disciplinary team

Leg Ulcer Hosiery Kits available:
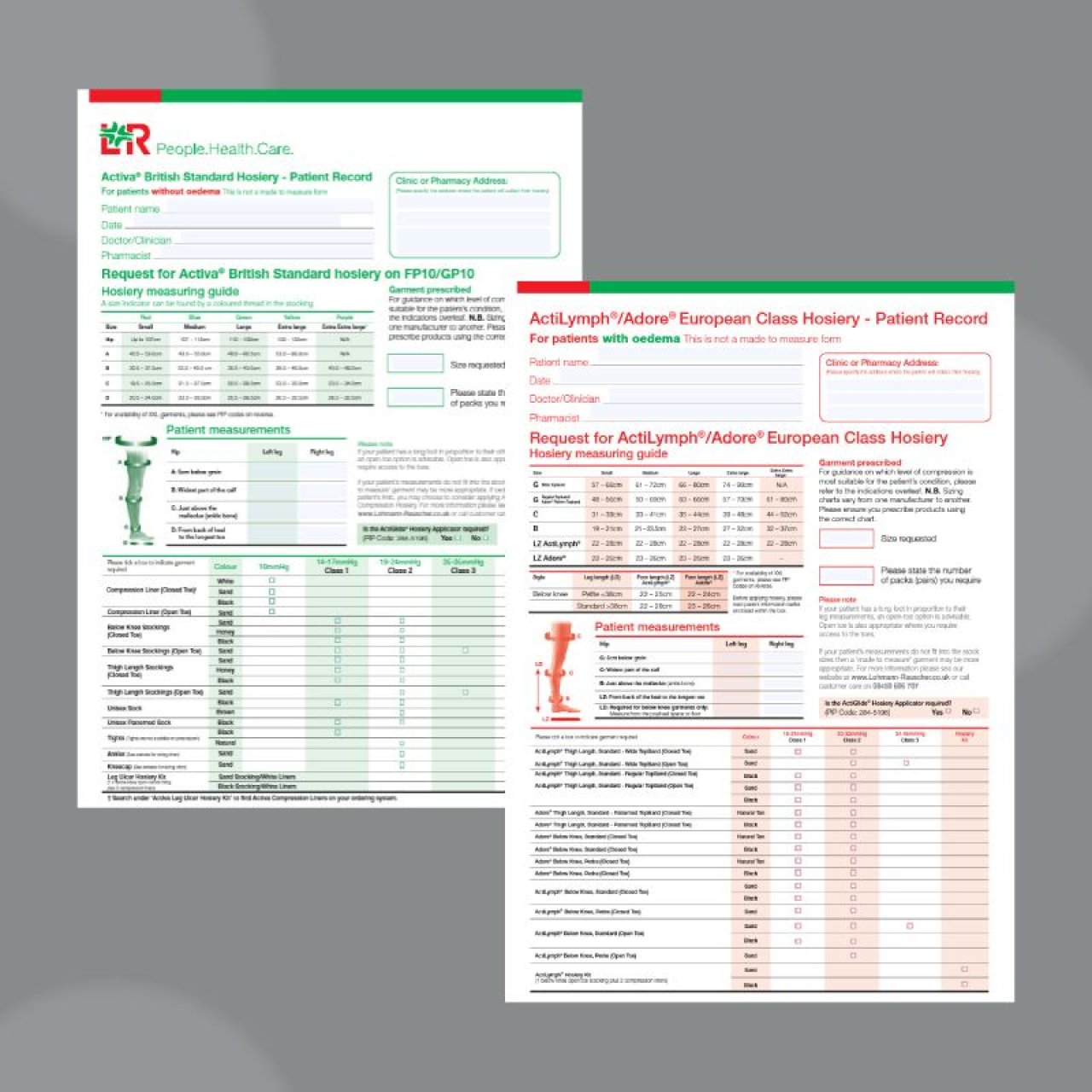
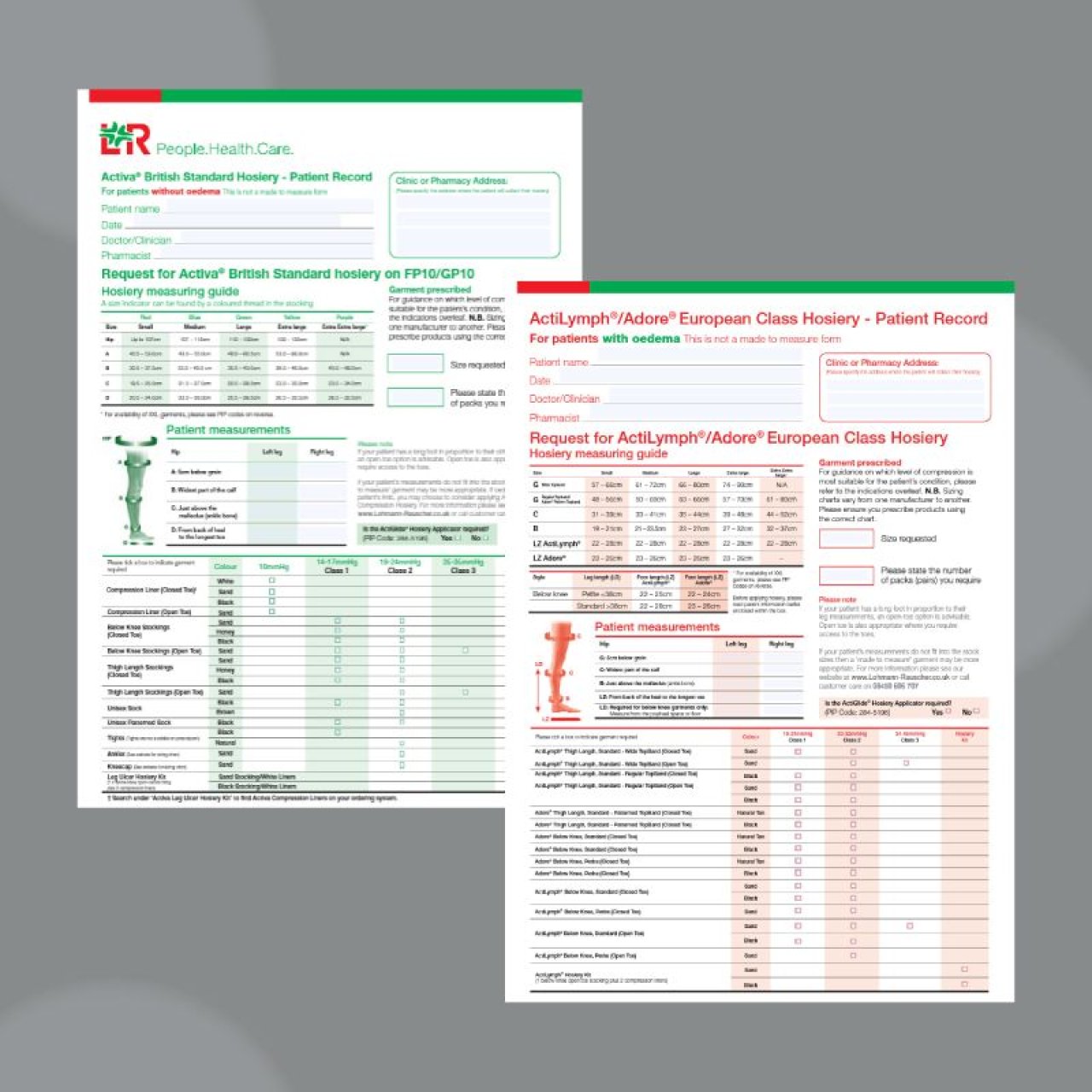
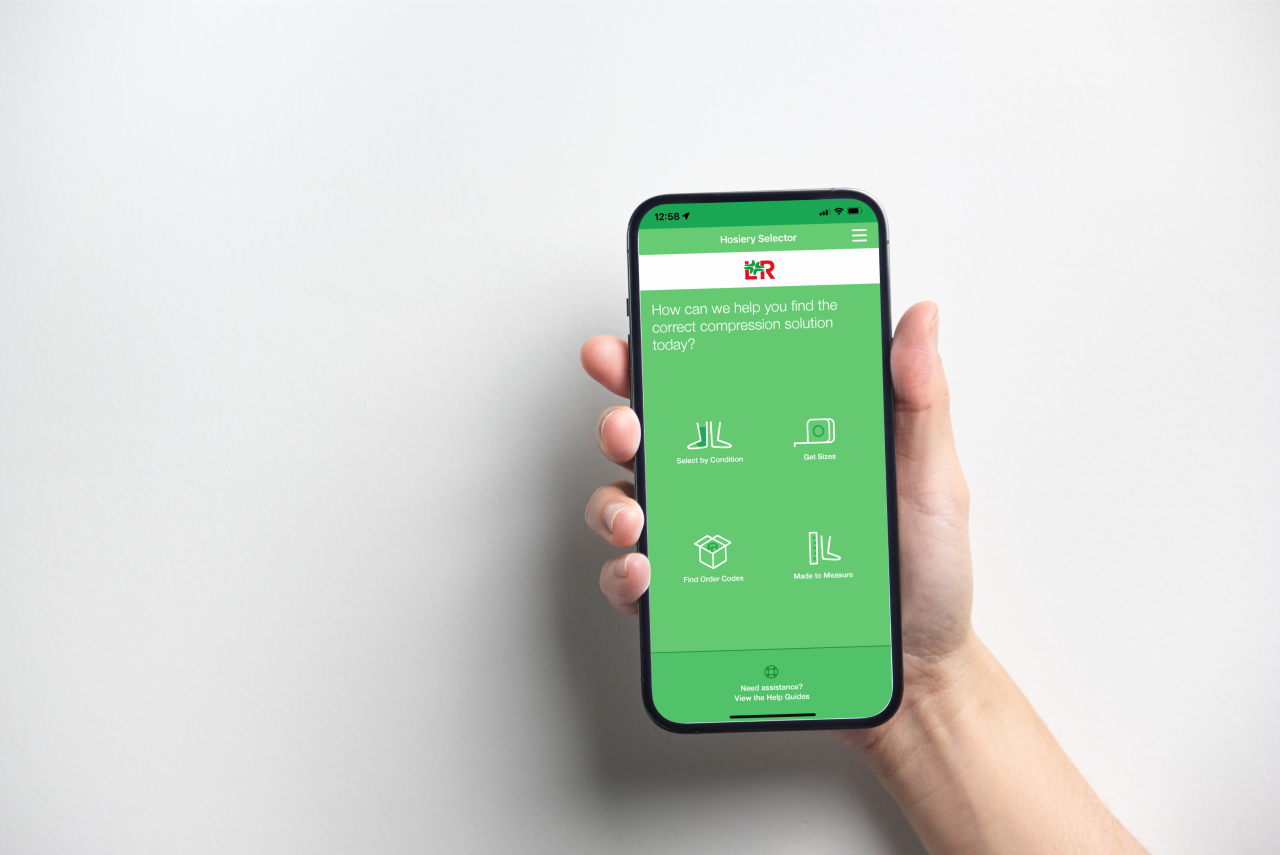
Activa Leg Ulcer Hosiery Kit - for the treatment of limbs without oedema
ActiLymph Leg Ulcer Hosiery Kit - for the treatment of limbs with oedema

What's contained within a Leg Ulcer Hosiery Kit:
Activa Leg Ulcer Hosiery Kit
x2 10mmHg liner
Open-toed British Standard Class 3 Stocking (25-35mmHg)
ActiLymph Leg Ulcer Hosiery Kit
x2 10mmHg liner
Open-toed European Classification Class 2 Stocking (23-32mmHg)
The two garments are worn together, liner followed by the open-toe compression stocking, to provide full therapeutic compression.
Activa® Leg Ulcer Hosiery Kit, ActiLymph® Hosiery Kit and Activa® 10mmHg Liners can be found under ‘Venous Ulcer Compression System’ in the Drug Tariff and are available on FP10/GP10